Urinary Bladder
The urinary bladder is a hollow, muscular, and distensible organ that sits on the pelvic floor. It stores urine from the kidneys before disposal by urination via the urethra.
A. Bladder Cancer
Every year, about 10,000 people in the UK are diagnosed with bladder cancer. Of these, 8 out of 10 (80%) are diagnosed with early bladder cancer. Bladder cancer risk increases as people get older. Smoking is one of the most common causes of bladder cancer.
Bladder cancer signs and symptoms may include:
- Blood in the urine (haematuria)
- Painful urination
- Pelvic pain
- If you have haematuria, your urine may appear bright red or cola-colored. Sometimes, blood in the urine can’t be seen and is picked up in a simple urine test. This is called non-visible or microscopic haematuria.
If you see blood in your urine, it’s very important to get it checked by your GP straight away.
People with bladder cancer might also experience:
- Back pain
- Frequent urination
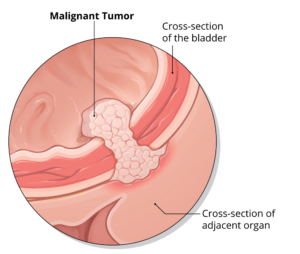
Types of Bladder Cancer
Bladder cancer may appear in different forms:
Transitional cell bladder cancer (TCC)
TCC, also known as urothelial carcinoma, is the most common type of bladder cancer. The cancer starts in cells in
the bladder lining (urothelium).
Some bladder cancers begin as an invasive tumour growing into the muscle wall of the bladder. Others begin at a
non-invasive stage that involves only the inner lining of the bladder – this is early (superficial) bladder cancer.
Carcinoma in situ (CIS) is a type of non-invasive bladder cancer that appears as a flat, red area in the bladder.
Rarer types of bladder cancer:
These include squamous cell cancer and adenocarcinoma. Squamous cell cancers start from another type of cell in
the bladder lining. Adenocarcinoma starts from glandular cells.
B. Interstitial Cystitis
Interstitial cystitis is a chronic condition causing bladder pressure, bladder pain and sometimes pelvic pain. The pain ranges from mild discomfort to severe pain. The condition is a part of a spectrum of diseases known as painful bladder syndrome.
Normally, the bladder expands until it’s full and then signals your brain that it’s time to urinate, communicating through the pelvic nerves. This creates the urge to urinate for most people.
With interstitial cystitis, these signals get mixed up — you feel the need to urinate more often and with smaller volumes of urine than most people.
Interstitial cystitis most often affects women and can have a long-lasting impact on quality of life. Although there’s no cure, medications and other therapies may offer relief.
C. Overactive bladder
Overactive bladder, also called OAB, causes a frequent and sudden urge to urinate that may be difficult to control. You may feel like you need to pass urine many times during the day and night, and may also experience unintentional loss of urine (urgency incontinence).
If you have an overactive bladder, you may feel embarrassed, isolate yourself, or limit your work and social life. The good news is that a brief evaluation can determine whether there’s a specific cause for your overactive bladder symptoms.
You may be able to manage symptoms of an overactive bladder with simple behavioral strategies, such as dietary changes, timed voiding and bladder-holding techniques using your pelvic floor muscles. If these initial efforts don’t help enough with your overactive bladder symptoms, additional treatments are available.
D. Urinary leakage
Urinary incontinence is when a person cannot prevent urine from leaking out.
It can be due to stress factors, such as coughing, it can happen during and after pregnancy, and it is more common with conditions such as obesity.
The chances of it happening increase with age.
Bladder control and pelvic floor, or Kegel, exercises can help prevent or reduce it.
